Back

Don’t let back
Back pain affects your entire outlook on life. It’s difficult to be active, almost impossible to get comfortable, and even harder to engage in the everyday activities most people take for granted.
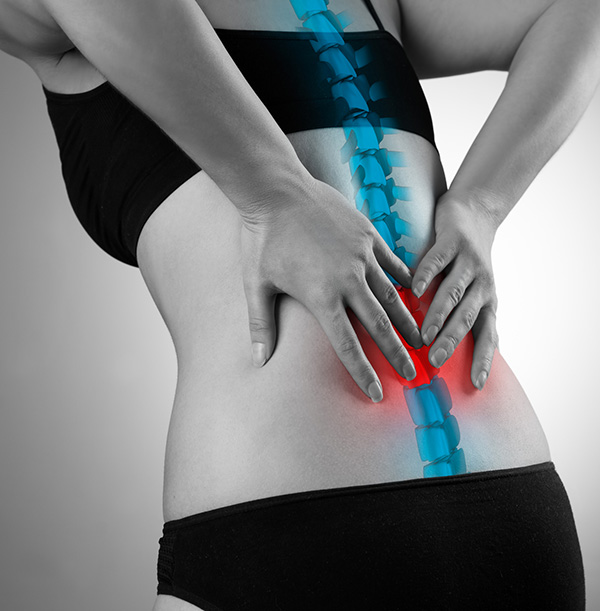
Pain in your back can be the result of conditions that affect the vertebrae of your thoracic spine (upper back) and/or lumbar spine (lower back), the discs between the vertebra, and/or the ligaments, spinal cord, and nerves around the area.
Many people believe they simply have to live with back pain, or are afraid they will have to have major surgery in order to relieve the pain. However, over the last few years, there have been numerous advancements in technology that make alleviating back pain less invasive than ever. Dr. Soldevilla uses these advanced treatment options so your pain will be alleviated and you can start living your life again.
The key to finding relief of your back pain is understanding the cause of your pain. Here are some of the most common causes of back pain, their symptoms, and their treatment:

Herniated
Disc
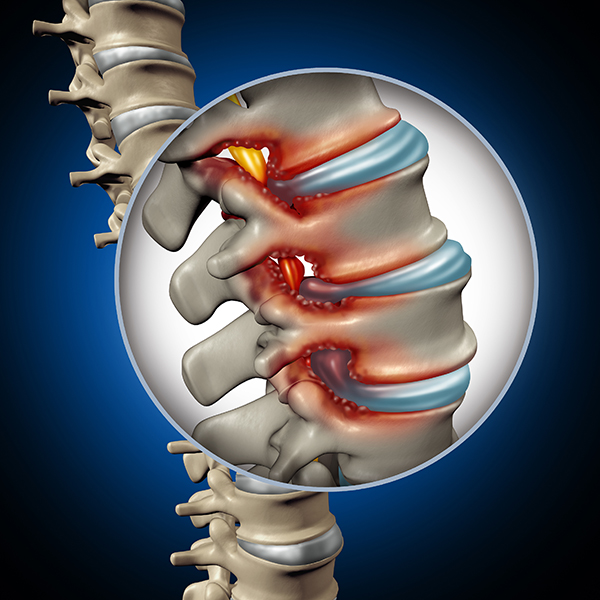
The term “herniated disc” refers to a problem with one of the rubbery, gel-like cushions between the vertebrae of the spine, in this case the lumbar spine (lower back). Disc herniation occurs when the interior “jelly” of the disc pushes through the tougher exterior and irritates nearby nerves, resulting in pain that ranges from mild to severe.
When a disc is herniated, it may bulge and the jelly-like interior could leak out through a tear, or the bulge may press against or pinch a nerve.
SYMPTOMS
Symptoms caused by a herniated disc in your lumbar spine include:
- Pain in your leg, especially in the buttocks, thigh, and calf
- Numbness or tingling in your leg
- Weakness of your leg
Pain is caused by inflammatory chemicals that are released around the injured area, and the injured disc can also put pressure on the nerve roots as they travel through the adjoining tunnel to and from the spinal cord. This can cause pain, pins and needles and numbness into your leg and also lead to significant muscular weakness.
TREATMENT
Most people with mild disc herniation will improve on their own in about six to eight weeks. For other people, the pain will be more intense and persistent and physical therapy may be indicated to help alleviate symptoms. Anti-inflammatory medication and pain relievers may also be necessary.
In a small group of people, symptoms don’t respond to conservative measures or time. When this is the case, Dr. Soldevilla may recommend surgery, particularly if there is persistent pain or weakness in your legs. When surgery is indicated, it is usually aimed at reducing the pressure from the herniated disc on surrounding tissues and is especially focused on relieving any pressure on the nerve roots as they exit from the spinal cord. This should relieve any pain or sensation traveling down into your legs.
Fortunately, recent technological advancements in spinal surgery have led to much less invasive procedures for disc herniation. Afterward, most patients enjoy a faster recovery.
There are several different types of surgical procedures for herniated discs. Dr. Soldevilla will discuss these procedures with you and together you will choose the one that is most suitable for you.
Radiculopathy
(Leg Pain, Sciatica)
Radiculopathy is the clinical term that describes a nerve root in the lumbar spine area becoming inflamed or damaged and causing pain and other symptoms in the buttock/leg/foot area. Also commonly known as sciatica, lumbar radiculopathy most commonly results from degenerative changes to the lumbar spine over long periods of time, but can also occur due to acute injury or illness.
SYMPTOMS
With lumbar radiculopathy, pain can radiate anywhere along the buttock/leg/foot area. Other symptoms in this area can include:
- Numbness
- Altered reflexes
- Weakness
- Tingling
TREATMENT
Radiculopathy of the back can be treated in a number of different ways, both surgical and non-surgical. Non-surgical treatments are typically the first line of treatment and can include:
- Rest or activity modification
- Physical therapy
- Ice and/or heat therapy
- Medication including over-the-counter anti-inflammatory drugs and/or pain relievers
- Manual manipulation
- Epidural steroid injection
If non-surgical treatments don’t provide the pain relief you are looking for, surgery could be the next step. There are a number of different surgical solutions, depending on the cause of the lumbar radiculopathy, and typically focus on decompressing the nerve and/or stabilizing the spine.


Degenerative
Disc Disease
Degenerative disc disease is a common condition among aging adults that refers to the process of degenerative changes that occur in the discs – the soft, gel-like pads located between the vertebrae of your spine. Wear and tear on your spine over time cause the discs to gradually lose their ability to cushion the vertebrae.
At the same time, the outer layer of the spine can develop cracks, which gradually worsen. The discs may also develop herniated areas, which is where the central portion of the disc protrudes through the outer layer.
SYMPTOMS
A lumbar disc herniation in the lower back may result in:
- Shooting pain into the buttocks or down the leg
- Local severe back pain or “burning” in the back
- Weakness in one or both legs
- Changes in bowel or bladder activity
- Lack of sensation or pins-and-needles tingling in one or both legs
Despite the fact that the physical degeneration in your spine will gradually progress over time, the good news is that your symptoms may not necessarily progress to the same extent. Sometimes, symptoms can even improve over time. A number of studies have shown that pain levels in this condition are actually worse in younger people than older. There are a few reasons why this may be so – the joints in the back tend to stiffen up with age, leading eventually to more stability; and also, the inflammatory chemicals that are contained within the nucleus pulposus can eventually become depleted.
For some people, however, particularly if the pain levels are severe, or if there is pressure on the nerve roots, symptoms will continue to escalate with time.
TREATMENT
Most people with degenerative disc disease respond well to conservative, non-surgical treatment. This conservative treatment typically includes anti-inflammatory medication and pain relievers. Physical therapy can help to manage your symptoms and may include manual therapy, heat and other pain-relieving methods, stretching, strengthening exercises and education to help you manage your condition.
For a small group of people who don’t respond to conservative treatment, surgery may be necessary, particularly if there are signs and symptoms of nerve compression or joint instability. There is a wide range of surgical techniques that may be used for this condition, depending on the extent and exact nature of the damage to the disc and spine. Dr. Soldevilla will discuss with you fully the type of surgery he recommends for you and will work with you to develop a treatment plan.
Spondylolisthesis
Spondylolisthesis is a common condition in which one vertebrae slips out of place and onto the vertebra below it and typically affects the vertebra of the lower back. If the vertebra slips too far, it may press on a nerve, which can cause pain and limitation.
The three most common forms of the condition are:
- Degenerative Spondylolisthesis is the most common form and happens with aging as the discs that cushion the vertebrae become less spongy.
- Congenital Spondylolisthesis occurs when an abnormal bone formation is present at birth.
- Isthmic Spondylolisthesis leads to small stress fractures in the vertebrae.
Less common are:
- Traumatic Spondylolisthesis occurs when an injury causes a spinal fracture.
- Pathological Spondylolisthesis occurs when a disease like osteoporosis, a tumor, or an infection weakens the spine.
- Post-Surgical Spondylolisthesis sometimes happens after spine surgery.
SYMPTOMS
Spondylolisthesis symptoms range from mild to severe. Depending on the severity of the condition, the following symptoms may be present:
- Pain in the lower back, often worse after walking or exercise, or extending the back (straightening or leaning back)
- Stiffness in the lower back
- Increased tightness of the hamstrings
- Pain, numbness, or tingling in your legs if nerves are being compressed
- Loss of control of bladder or bowel function (in severe cases)
TREATMENT
Dr. Soldevilla will first carry out a thorough assessment to determine the severity of your condition. Spondylolisthesis will usually be evident on plain x-rays but further scans such as an MRI or CT scan may be ordered to see if there is pressure on other structures, such as nerves or the spinal cord.
In less severe cases, physical therapy may be helpful. This treatment may consist of manual therapy, stretches to address the tightness of hamstrings and other structures, and strengthening exercises for your core muscles to help support your back. Your doctor may also prescribe medication to help manage your pain and reduce inflammation. A back brace is sometimes used to stabilize the area.
For a number of people with more severe forms of spondylolisthesis, surgery is recommended, especially if the slippage is severe or if there is pressure on the spinal cord or nerves. The goal of surgery is to provide more space for the spinal cord and nerve roots while stabilizing the spine. In some cases, it can also be effective at reducing pain. Dr. Soldevilla will discuss with you the most appropriate surgical technique for your condition.
Spinal
Stenosis
Spinal stenosis of the back is usually a slow process that occurs over years results in thickening of the ligaments, formation of bone spurs, and deterioration of the disc material. As a result, the spinal canal narrows and pinches the nerves. Bone spurs may also press on the spinal cord.
Lumbar Stenosis may produce lower back pain and leg discomfort or pain. Surgery may be necessary if lumbar stenosis limits normal activity, causes leg weakness and/or numbness, makes standing or walking difficult, or affects your ability to control of bowel and bladder functions.
Thoracic Stenosis – The thoracic spine in the upper back has some unique characteristics that make thoracic spinal stenosis a little different than stenosis in other areas. Because the 12 thoracic vertebrae connect to the 12 sets of ribs that protect our major organs, the thoracic spine is more fixed than the cervical or lumbar areas. The spinal canal is narrower than the rest of the spine, too. Thoracic stenosis typically is accompanied by stenosis in the lumbar area and sometimes also the cervical spine.
SYMPTOMS
Symptoms may include:
- Back pain
- Radiating pain into the legs, especially when moving
- Leg weakness and/or numbness
- Difficulty standing or walking
- Change in bowel or bladder function
TREATMENT
Often, a conservative treatment of physical therapy, anti-inflammatory medication, and/or pain relievers may be sufficient to alleviate symptoms of stenosis.
However, Dr. Soldevilla will typically recommend surgery if there are signs that the spinal cord or nerves are compressed. Surgery is necessary if neurological symptoms increase, such as difficulty with balance or walking.
If Dr. Soldevilla feels surgery is your best option, he will take the least invasive approach he can that will give you the optimal outcome, and will fully discuss his recommended procedure with you.

Synovial
Cyst
A synovial cyst is a benign, fluid-filled sac that develops as a result of degeneration of the spine. The sac creates pressure inside the spinal canal, compressing the nerves and causing numbness, stiffness, weakness, and pain, especially when the patient is active. A synovial cyst is an uncommon cause of spinal stenosis in the lumbar part of the spine (lower back).
Because a synovial cyst develops from degeneration of the spine, it is most common in people over 65 years of age, and rarely seen in anyone under 45 years of age.
SYMPTOMS
Symptoms may include:
- Pain in the lower back
- Pain in one or both legs
- Pain that radiates down the back of the leg and to the feet
- Leg cramps
- Tingling or numbness in one or both legs
- Increased symptoms when standing that eases when sitting
TREATMENT
Patients with synovial cysts can often control their symptoms through activity modification, non-surgical treatment for pain relief (i.e. NSAIDS, pain relievers), injections, and/or physical therapy.
Dr. Soldevilla may recommend surgery if there are signs that the spinal cord is compressed or there is significant risk that the spinal cord may become damaged. Surgery is necessary if neurological symptoms increase, such as difficulty with balance or walking.
The most reliable kind of spine surgery for synovial cysts is decompression surgery combined with spinal fusion, during which the cyst is removed and, occasionally, the joint fused. Once the joint is fused, all motion is stopped in that particular area, so the cyst is unlikely to regenerate.

